
Celiac disease is a serious auto-immune disorder that affects over 3 million Americans and may have serious implications—-unfortunately, most patients are never diagnosed.
If you have celiac disease, eating gluten triggers an immune response in your small intestine and causes inflammation. Overtime, the intestinal damage can cause weight loss, bloating and sometimes diarrhea.
Eventually, your brain, nervous system, bones, liver and other organs can be deprived of vital nourishment.
The following article helps patients understand this disease and provides information about how to prevent the detrimental effects of this disease.
The signs and symptoms of celiac disease can vary greatly.
Although the classic signs are diarrhea and weight loss, most people with celiac disease experience few or no digestive signs or symptoms. Only about one-third of people diagnosed with celiac disease experience diarrhea, and about half have weight loss.
Twenty percent of people with celiac disease have constipation, and 10 percent are obese.
In addition to digestive problems, other signs and symptoms of celiac disease include:
- Anemia, usually resulting from iron deficiency
- Loss of bone density (osteoporosis) or softening of bone (osteomalacia)
- Itchy, blistery skin rash (dermatitis herpetiformis)
- Damage to dental enamel
- Headaches and fatigue
- Nervous system injury, including numbness and tingling in the feet and hands, and possible problems with balance
- Joint pain
- Reduced functioning of the spleen (hyposplenism)
- Acid reflux and heartburn
As many as 75 percent of children with celiac disease are overweight or obese. Digestive signs and symptoms are experienced by 20 to 30 percent of children with the condition although the precise signs and symptoms differ by age.
In infants, typical signs and symptoms of celiac disease include:
- Chronic diarrhea
- Swollen belly
- Pain
- Failure to thrive or weight loss
Older children may experience:
- Diarrhea
- Constipation
- Short stature
- Delayed puberty
- Neurologic symptoms, including attention-deficit/hyperactivity disorder (ADHD), learning disability, headaches and lack of muscle coordination
Dermatitis herpetiformis is an itchy, blistering skin disease that stems from intestinal gluten intolerance. The rash usually occurs on the elbows, knees, torso, scalp and buttocks.
Dermatitis herpetiformis is often associated with changes to the lining of the small intestine identical to that of celiac disease, but the disease may not produce noticeable digestive symptoms.
Dermatitis herpetiformis is treated with a gluten-free diet and medication to control the rash.
The precise cause of celiac disease isn’t known.
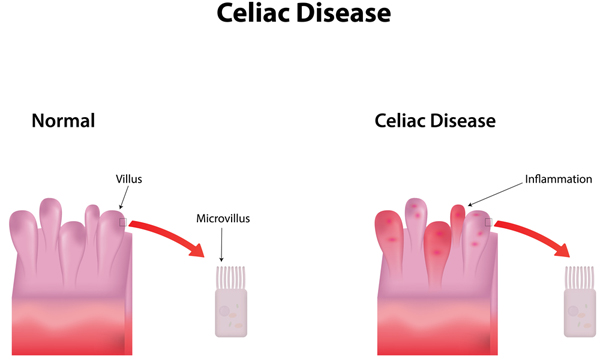
When the body’s immune system overreacts to gluten in food, the immune reaction damages the tiny, hair-like projections (villi) that line the small intestine. Villi absorb vitamins, minerals and other nutrients from the food you eat. Normally, villi resemble the deep pile of a plush carpet, on a microscopic scale. The damage resulting from celiac disease makes the inner surface of the small intestine appear more like a tile floor. As a result your body is unable to absorb nutrients necessary for health and growth.
A study done by Mayo Clinic and the National Institutes of Health estimates that about 1 in 141 people
in the U.S. have celiac disease, although the disease of- ten goes undiagnosed. Celiac disease is most common in Caucasians.
Some gene changes (mutations) appear to increase the risk of developing the disease. But having those gene mutations doesn’t mean you’ll get celiac disease — meaning other factors must be involved.
Sometimes celiac disease is triggered — or becomes active for the first time — after surgery, pregnancy, child- birth, viral infection or severe emotional stress.
Celiac disease can affect anyone. However, it tends to be more common in people who have:
- A family member with celiac disease or dermatitis herpetiformis
- Down syndrome or Turner syndrome
- Type 1 diabetes
- Autoimmune thyroid disease
- Sjögren’s syndrome
- Microscopic colitis (lympho- cytic or collagenous colitis)
Untreated, celiac disease can cause:
Malnutrition. The damage to your small intestine means it can’t absorb enough nutrients. Malnutrition can lead to anemia and weight loss. In children, malnutrition can cause stunted growth and delayed development.
Loss of calcium and bone density. Malabsorption of calcium and vitamin D may lead to a softening of the bone (osteomalacia or rickets) in children and a loss of bone density (osteoporosis) in adults.
Infertility and miscarriage. Malabsorption of calcium and vitamin D can contribute to reproductive issues.
Lactose intolerance. Damage to your small intestine may cause you to experience abdominal pain and diarrhea after eating lactose-containing dairy products, even though they don’t contain gluten. Once your intestine has

healed, you may be able to tolerate dairy products again. However, some people continue to experience lactose in- tolerance despite successful management of celiac disease.
Cancer. People with celiac disease who don’t maintain a gluten-free diet have a greater risk of developing several forms of cancer, including intestinal lymphoma and small bowel cancer.
You may be referred to a doctor who treats digestive diseases (gastroenterologist).
Tests and procedures used to diagnose celiac disease include:
Blood tests. Elevated levels of certain substances in your blood (antibodies) indicate an immune reaction to gluten. These tests detect celiac disease even if you have only mild symptoms or none at all.
Endoscopy. If your blood tests indicate celiac disease, your doctor may order an endoscopy to view your small intestine and to take a small tissue sample (biopsy) to analyze for damage to the villi.
It’s important to be tested for celiac disease before trying a gluten-free diet. Eliminating gluten from your diet may change the results of blood tests so that they appear to be normal.
A gluten-free diet is essential, and the only treatment for managing celiac disease. In addition to wheat, foods that contain gluten include:
- Barley
- Bulgur
- Durum
- Farina
- Graham flour
- Malt
- Rye
- Semolina
- Spelt (a form of wheat)
- Triticale
Your doctor may refer you to a dietitian, who can help you plan a healthy gluten-free diet.
Once gluten is removed from the diet, inflammation in the small intestine generally begins to lessen — usually within several weeks, though you may start to feel better in just a few days. Complete healing and regrowth of the villi may take several months to several years. Healing in the small intestine tends to occur more quickly in children than adults.
If you accidentally eat a product that contains gluten, you may experience abdominal pain and diarrhea. Some people experience no signs or symptoms after eating gluten, but this doesn’t mean it’s not harmful. Even trace

amounts of gluten in your diet can be damaging, whether or not they cause signs or symptoms.
If your nutritional deficiencies are severe, your doctor or dietitian may recommend taking vitamin and mineral supplements. You may need to supplement your levels of:
- Calcium
- Folate
- Iron
- Vitamin B-12
- Vitamin D
- Vitamin K
- Zinc
Vitamin supplements are usually taken in pill form. If your digestive tract has trouble absorbing vitamins, your doctor may give them by injection.
If you have this itchy, blistering skin rash that some- times accompanies celiac disease, your doctor may recommend a skin medication (dapsone) along with the gluten- free diet.
Packaged foods should be avoided unless they’re labeled as gluten-free or have no gluten-containing ingredients. In addition to cereals, pastas and baked goods — such as breads, cakes, pies and cookies — other packaged foods that may contain gluten include:
- Beer
- Candies
- Gravies
- Imitation meats or seafood
- Processed luncheon meats
- Salad dressings and sauc- es, including soy sauce
- Self-basting poultry
- Soups
- Certain grains*
*Certain grains, such as oats, can be contaminated with wheat during growing and processing. It’s not clear whether oats are harmful for most people with celiac disease, but
doctors generally recommend avoiding oats unless they are specifically labeled gluten-free. Occasionally, even pure oats can be a problem for people with celiac disease.
Many basic foods are allowed in a gluten-free diet, including:
- Fresh meats, fish and poultry that aren’t breaded, batter-coated or marinated
- Fruits
- Most dairy products
- Potatoes
- Vegetables
- Wine and distilled liquors, ciders and spirits
Grains and starches allowed in a gluten-free diet include:
- Amaranth
- Arrowroot
- Buckwheat
- Corn
- Cornmeal
- Gluten-free flours (rice, soy, corn, potato, bean)
- Pure corn tortillas
- Quinoa
- Rice
- Tapioca
Fortunately for bread and pasta lovers with celiac dis- ease, an increasing number of gluten-free products are available. If you can’t find any at your local bakery or grocery store, check online. There are gluten-free substitutes for many gluten-containing foods.





