or millions of Americans, back pain is a daily fact of life. Many blame aging as the cause, but for more than 700,000 women and men, the real culprit is vertebral compression fractures (VCFs) caused by osteoporosis. In fact, VCFs are the most common complication from osteoporosis and often result in prolonged disability. Back pain can be a surface symptom of a much deeper problem, namely osteoporosis.
According to the National Osteoporosis Foundation, fractures from osteoporosis are about twice as common in women as they are in men. The following article provides information about the risk factors for osteoporosis, preventative measures and effective treatments that will help patients who suffer from this condition.
- Increasing age
- Small frame or low body weight
- Caucasian or Asian ethnicity
- Family history of osteoporosis
- Low levels of sex hormones
- Diet low in calcium and vitamin D
- Sedentary lifestyle
- Hyperthyroidism
- Heavy use of alcohol
- Cigarette smoking
You can’t feel yourself losing bone, but you might feel a spinal fracture—the most common complication from osteoporosis.2,3,5 Acute and chronic back pain are outward signs of such fractures (also known as vertebral compression fractures or VCFs5 ). It may be hard to believe, but even simple activities like carrying groceries or bending over to pick up your grandchild can cause a VCF.5,6,7
Your spine is stacked and structured with the precision of dominoes, allowing you to bend over and twist side to side. And just like dominoes, one VCF can change your spine’s alignment and cause other vertebrae to collapse and fracture. Multiple fractures may lead to loss of height and curvature of the upper back called kyphosis or “dowager’s hump.”8 Over time, kyphosis can cause your back to hunch over so badly it reduces the space in your chest cavity, making it hard to breathe and eat.5
Don’t lightly dismiss new or unusual back pain as a part of growing old. Your back- ache could be a VCF. Sudden and severe pain or pain that lasts more than a week should be seen by a doctor.
You can’t feel yourself losing bone, but you might feel a spinal fracture—the most common complication from osteoporosis.2,3,5 Acute and chronic back pain are outward signs of such fractures (also known as vertebral compression fractures or VCFs5 ). It may be hard to believe, but even simple activities like carrying groceries or bending over to pick up your grandchild can cause a VCF.5,6,7
Your spine is stacked and structured with the precision of dominoes, allowing you to bend over and twist side to side. And just like dominoes, one VCF can change your spine’s alignment and cause other vertebrae to collapse and fracture. Multiple fractures may lead to loss of height and curvature of the upper back called kyphosis or “dowager’s hump.”8 Over time, kyphosis can cause your back to hunch over so badly it reduces the space in your chest cavity, making it hard to breathe and eat.5
Don’t lightly dismiss new or unusual back pain as a part of growing old. Your back- ache could be a VCF. Sudden and severe pain or pain that lasts more than a week should be seen by a doctor.
to support the spine, and even weakened arches, which flat- ten feet and contribute slightly to height loss. The good news is that a diet with enough calcium and vitamin D, together with weight-bearing exercise, can spare your spine from significant height loss.5,9,10
Weight-bearing exercise reduces bone loss and helps prevent fractures. Activities such as walking, running, climbing stairs, tennis, and weight lifting put stress on your bones, signaling your body that your bones need to be made stronger. New cells are added to strengthen your bones. That’s why if you’re right-handed, the bones on your right arm are slightly larger and stronger—it’s from extra use. To get the bone- building benefit from exercise, you must do it at least three times per week for 30-45 minutes.9,5
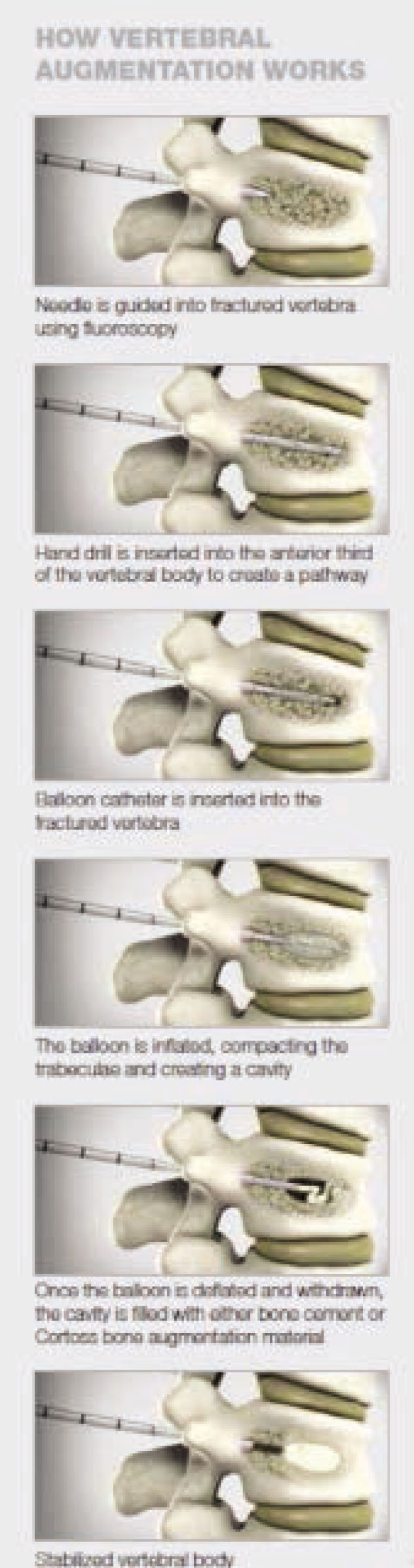
Until about 20 years ago, doctors were limited in how they could treat VCFs. Pain medications, bed rest, bracing, and physical therapy were the only options available outside of major spine surgery. Though many of these options are still the first line of defense,5,22 today there is a safe and effective treatment called vertebral augmentation, a minimally invasive procedure proven to significantly relieve pain, in- crease mobility, and improve quality of life without open surgery.14,15,16,17,18,19,20,21
VERTEBRAL AUGMENTATION is performed by specialists including interventional pain management physicians. During the procedure, one or two balloons are used to create a void or cavity in the collapsed vertebra into which an injected material—either bone cement or Cortoss bone augmentation material—is introduced. The hardened cement creates an internal cast that stabilizes the fracture, thereby alleviating the pain in approximately 90 percent of patients.2,21
Performed through a small incision in the back, vertebral augmentation can be done on an outpatient basis and usually requires only a local anesthetic and mild sedation, eliminating the possible complications that may result from open surgery.
- Rapid and Sustained Pain Relief14-21
- Increased Mobility14-21
- Improved Quality of Life14-17,21
- Low Complication Rate14,15,21
Women who can’t get out of a chair without using their arms have twice the fracture risk of those who can stand up effortlessly.11
You’re never too old—or too young—to improve your bone health. There are many things that you can do to keep your bones strong and prevent fractures. A diet rich in calcium and weight-bearing exercise can prevent osteoporosis.9 So can talking to your doctor. Schedule an appointment to- day to discuss ways to protect your bones and treat bone- related problems such as vertebral compression fractures.
Calcium-rich foods are the secret to maintaining bone strength. Women aged 50 and under need 1,000 milligrams a day. After age 50, daily requirements jump to 1,200 milligrams8 Lack of calcium has been singled out as a major public health concern because it is critically important to bone health. The average American consumes far less than the amount required. Calcium supplements are a good way to make up the difference.9 How does your diet measure up?
Here are some good sources of calcium:12
- 8 oz. low-fat yogurt: 415mg calcium
- 16 oz. milkshake: 380mg calcium
- 24 almonds: 75mg calcium
- 1 oz. cheddar cheese: 204mg calcium
- 8 oz. 1% milk: 305mg calcium
- 1 cup spinach (frozen, cooked): 291mg calcium
- 1 cup Total Raisin Bran® cereal: 1038mg calcium




