
Gastroesophageal reflux disease (GERD) is a chronic digestive disease that occurs when stomach acid or, occasionally, bile flows back (refluxes) into your food pipe (esophagus). The backwash of acid irritates the lining of your esophagus and causes GERD signs and symptoms.
Signs and symptoms of GERD include acid reflux and heartburn. Both are common digestive conditions that many people experience from time to time. When these signs and symptoms occur at least twice each week or interfere with your daily life, doctors call this GERD.
Most people can manage the discomfort of heartburn with lifestyle changes and over-the-counter medications. But for people with GERD, these remedies may offer only temporary relief. People with GERD may need stronger medications, even surgery, to reduce symptoms.
GERD signs and symptoms include:
- A burning sensation in your chest (heartburn), sometimes spreading to the throat, along with a sour taste in your mouth
- Chest pain
- Dry cough
- Difficulty swallowing (dysphagia)
- Hoarseness or sore throat
- Regurgitation of food or sour liquid (acid reflux)
- Sensation of a lump in the throat
When to See a Doctor: Seek immediate medical attention if you experience chest pain, especially when accompanied by other signs and symptoms, such as shortness of breath or jaw or arm pain. These may be signs and symptoms of a heart attack.
GERD is caused by frequent acid reflux—the backup of stomach acid or bile into the esophagus.
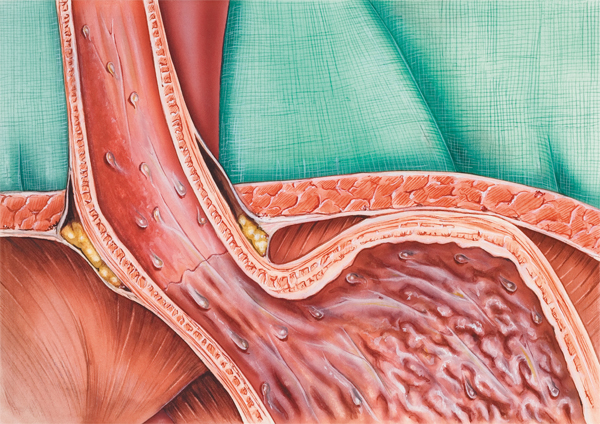
When you swallow, the lower esophageal sphinctera circular band of muscle around the bottom part of your esophagus—relaxes to allow food and liquid to flow down into your stomach. Then it closes again.
However, if this valve relaxes abnormally or weakens, stomach acid can flow back up into your esophagus, causing frequent heartburn and disrupting your daily life. This constant backwash of acid can irritate the lining of your esophagus, causing it to become inflamed (esophagitis).
Over time, the inflammation can erode the esophagus, causing complications such as bleeding or breathing problems.
Conditions that can increase your risk of GERD include:
- Obesity
- Hiatal hernia
- Pregnancy
- Smoking
- Dry mouth
- Asthma
- Diabetes
- Delayed stomach emptying
- Connective tissue disorders, such as scleroderma
- Zollinger-Ellison syndrome
Over time, chronic inflammation in your esophagus can lead to complications, including:
- Narrowing of the esophagus (esophageal stricture)
- An open sore in the esophagus (esophageal ulcer)
- Precancerous changes to the esophagus (Barrett’s esophagus)
If you’re bothered by frequent heartburn or other signs and symptoms, your doctor may be able to diagnose GERD with that information alone. Your doctor may also suggest tests and procedures used to diagnose GERD, including an endoscopy by a specialist who passes a flexible camera tube down your throat to evaluate the upper part of your digestive system. Your doctor may also use endoscopy to collect a sample of tissue (biopsy) for further testing. Endoscopy is useful in looking for complications of reflux, such as Barrett’s esophagus.
Treatment for heartburn and other signs and symptoms of GERD usually begins with over-the-counter medications that control acid. If you don’t experience relief within a few weeks, your doctor may recommend other treatments, includ- ing medications and surgery.
Over-the-counter treatments that may help control heartburn include:
- Antacids that neutralize stomach acid.Antacids, such as
Maalox, Mylanta, Gelusil, Rolaids, and Tums, may provide quick relief. But antacids alone won’t heal an inflamed esophagus dam- aged by stomach acid. Overuse of some antacids can cause side effects, such as diarrhea or constipation.
- Medications to reduce acid production.Called H-2- receptor blockers, these medications include cimetidine (Tagamet HB), famotidine (Pepcid AC), nizatidine (Axid AR), or ranitidine (Zantac 25, Zantac 75, Zantac 150). H-2-receptor blockers don’t act as quickly as antacids, but they provide longer relief. Stronger versions of these medications are available in prescription form.
- Medications that block acid production and heal the
esophagus.Proton pump inhibitors block acid production and allow time for damaged esophageal tissue to heal. Over-the- counter proton pump inhibitors include lansoprazole (Prevacid 24 HR) and omeprazole (Prilosec OTC).
Contact your doctor if you need to take these medications two or more times a week or if your symptoms are not relieved. GERD medications are sometimes combined to increase effec- tiveness.
Most GERD can be controlled through medications. In situations where medications aren’t helpful or you wish to avoid long-term medication use, your doctor may recommend a more invasive procedure, such as a surgery to reinforce the lower esophageal sphincter (Nissen funfoplication).
Lifestyle changes may help reduce the frequency of heartburn. Consider trying to:
- Maintain a healthy weight.Excess pounds put pressure on your abdomen, pushing up your stomach and causing acid to back up into your esophagus. If your weight is healthy, work to maintain it. If you are overweight or obese, work to slowly lose weight—no more than 1 or 2 pounds (0.5 to 1 kilogram) a week. Ask your doctor for help in devising a weight-loss strategy that will work for you.
- Avoid tight-fitting clothing.Clothes that fit tightly around your waist put pressure on your abdomen and the lower esophageal sphincter.
- Avoid foods and drinks that trigger heartburn.Everyone has specific triggers. Common triggers such as fatty or fried foods, tomato sauce, alcohol, chocolate, mint, garlic, onion, and caffeine may make heartburn worse. Avoid foods you know will trigger your heartburn.
- Eat smaller meals.Avoid overeating by eating smaller
meals. - Don’t lie down after a meal.Wait at least three hours after eating before lying down or going to bed.
- Elevate the head of your bed.If you regularly experience heartburn at night or while trying to sleep, put gravity to work for you. Place wood or cement blocks under the feet of your bed so that the head end is raised by six to nine inches. If it’s not possible to elevate your bed, you can insert a wedge between your mattress and box spring to elevate your body from the waist up. Wedges are available at drugstores and medical supply stores. Raising your head with additional pillows is not effective.
- Don’t smoke.Smoking decreases the lower esophageal sphincter’s ability to function properly.
Adapted from the MayoClinic.com article “GERD “ (http://www.mayoclinic.com/health/gerd/DS00967) © Mayo Foundation for Medical Education and Research. All rights reserved.



