laucoma is an eye disease that causes damage to the optic nerve, usually due to high pressure within the eye. Because the optic nerve transmits sight to the brain, this damage can cause permanent loss of vision. It is pain- less, progressive, and can lead to total blindness
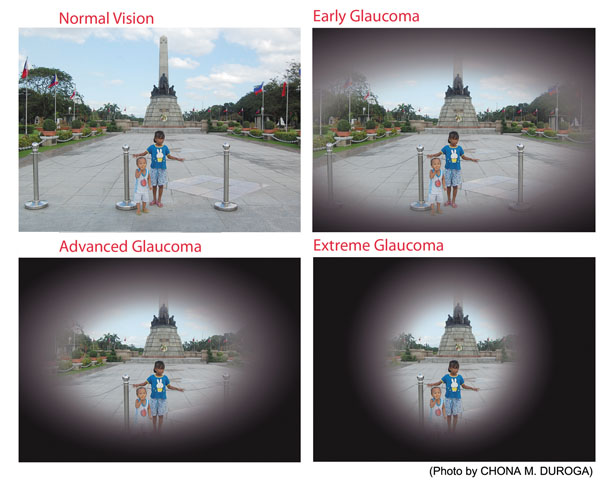
Open-angle Glaucoma is the most common form. This type occurs when there is resistance to the drainage of the aqueous humor. As this resistance increases, the IOP of the eye gradually increases. This rise in pressure con- tinues unchecked until it is too high for the nerves to tolerate and they start to die off. When a nerve dies, it cannot regenerate. It is a permanent loss. Fortunately we have many more nerves in the eye than needed and so the loss of nerves is not noticed immediately. Gradually, the peripheral vision has small areas of visual loss, which then get larger and larger until there is only a small amount of vision remaining. If it is not taken care of, complete blind- ness will result. All of this takes place usually over many years and there is no pain. That is also why it is hard to know if you have vision loss; it happens so slowly that you do not notice the difference.
It is very rare but needs to be addressed quickly to save vision. Secondary glaucomas are the type that arise due to some other eye condition or disease. These can happen due to trauma, bleeding within the eye, large cataracts, or the use of steroid eye drops.
RISK FACTORS: Specific risk factors include: age, family history of glaucoma, African or Hispanic ancestry, near and farsightedness, previous trauma, elevated IOP, low blood pressure, and not having the recommended eye exams.
SYMPTOMS: For the most common type of glaucoma, there are no symptoms. That is why regular eye exams are so important. For the other types, the symptoms are usually very obvious, such as severe pain or previous trauma.
DIAGNOSIS: Diagnosis comes from an eye exam.
- We test the pressure of the eye (IOP). Normal IOP is between 10-21 mmHg (millimeters of mercury). In angle closure it can get as high as 70 mmHg.
Closed-angle Glaucoma is a less common form. In this type of glaucoma, the IOP raises quickly due to sudden blockage of the drainage area of the eye. This quick rise results in blurry vision, extreme pain with headache and vomiting, red eyes, and a swollen cornea, the clear window of the eye. This is a medical emergency and must be treated immediately. People who experience this type of glaucoma don’t have any warning that the attack is coming. This is the type of glaucoma we are worried about happening with the use of over-the-counter decongestants.
Other Glaucoma – These include congenital glaucomas that babies are born with. They will have large irises (the colored part of the eye) and slightly bluish-colored corneas.
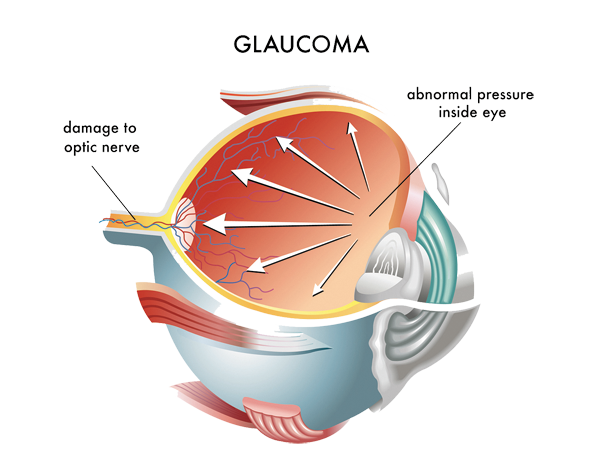
- We also look at the optic nerve. When there is damage to the optic nerve, it develops a characteristic look called “cupping.” We follow the amount of cupping to determine if the glaucoma progresses.
- Gonioscopy allows us to look at the drainage area of the eye. If we see the drain, it is open-angle; if we cannot, it is closed-angle.
- Testing of the peripheral vision allows us to see if any damage to the vision has occurred. These may be very small areas—too small for you to notice, but they show up on formal testing. These areas are watched closely for progression.
- Nerve fiber thickness testing lets us see if the nerves are becoming thinner gradually due to IOP that is too high.
- Corneal thickness measurement—those with thinner corneas are at higher risk of developing glaucoma.
TREATMENT: There are different types of treatment for dif- ferent types of glaucoma. The main goal is to lower the IOP.
- Medication in the form of eye drops is often the first treatment to be prescribed. These drops help the eye by either decreasing the amount of fluid produced or increasing the drainage of the fluid. Often these types of drops are used together in lowering the IOP to what is called the “Target Pressure.” This target pressure is different for each patient, depending upon their situation, and is set to a level that keeps damage from con- tinuing. Sometimes up to four eye drops are prescribed to keep the IOP in the target range. These drops will need to be taken for the rest of your life. It is very important not to miss a dose.
- Laser surgery can be utilized to decrease the pressure as well. The laser cleans out the drainage area of the eye, allowing the fluid to drain more easily, thus reduc- ing the IOP. New lasers can sometimes be used first
instead of medicine and reduce the need for eye drops for up to 5 years. It is painless and takes just a few minutes. It can be repeated if necessary to lower the IOP if it rises again. Another type of laser is used for angle closure glaucoma that dramatically reduces the IOP in a few minutes. It is used either emergently or to prevent an acute attack.
- Surgery: There are many types of surgeries to reduce the IOP. These are usually not used unless the laser treatment or eye drops don’t keep the pressure within the target range. There are types that cut a hole in the drainage area, place objects in the drain, peel the drain open, or remove parts of the drain. The type and severity of the glaucoma determines what is used.
- Marijuana: The American Academy of Ophthalmology says that even though marijuana has a temporary lowering effect on the IOP, it is not sustained long enough to treat glaucoma. Also, the drawbacks of smoking marijuana, including impaired functioning, pose too great a risk to be an adequate treatment.
The important take-away point about glaucoma is that it can occur in almost anyone at almost any time but becomes more likely as you age. If any of the risk factors present, get an eye exam. This can help save vision that would otherwise be lost. Today’s technology allows us to treat glaucoma with better and easier medicines, lasers, and surgery so that the number of people losing vision to this silent stealer of sight is much less than in the past. The future also holds many exciting developments.



